AC-YES
AC-YES
ACS Calculator: Your Evaluation Simplified
ACS Calculator: Your Evaluation Simplified
Beta Version - Under Construction - feedback welcomed
Beta Version - Under Construction - feedback welcomed
Instructions:
Best use case: Score after initial encounter (HPI, PE, ECG) prior to further results.
A score of 3+ is considered a rule in for ACS anything less necessitates modifiers, which add additional points, for rule in.
Note: A score of 2 places highest priority of rapidly evaluating for potential modifiers
This tool is dynamic. Significant changes in ECG or Clinical Picture necessitate fresh scoring from step one.
Instructions:
Best use case: Score after initial encounter (HPI, PE, ECG) prior to further results.
A score of 3+ is considered a rule in for ACS anything less necessitates modifiers, which add additional points, for rule in.
Note: A score of 2 places highest priority of rapidly evaluating for potential modifiers
This tool is dynamic and significant changes in ECG or Clinical Picture necessitate a fresh scoring from step one.
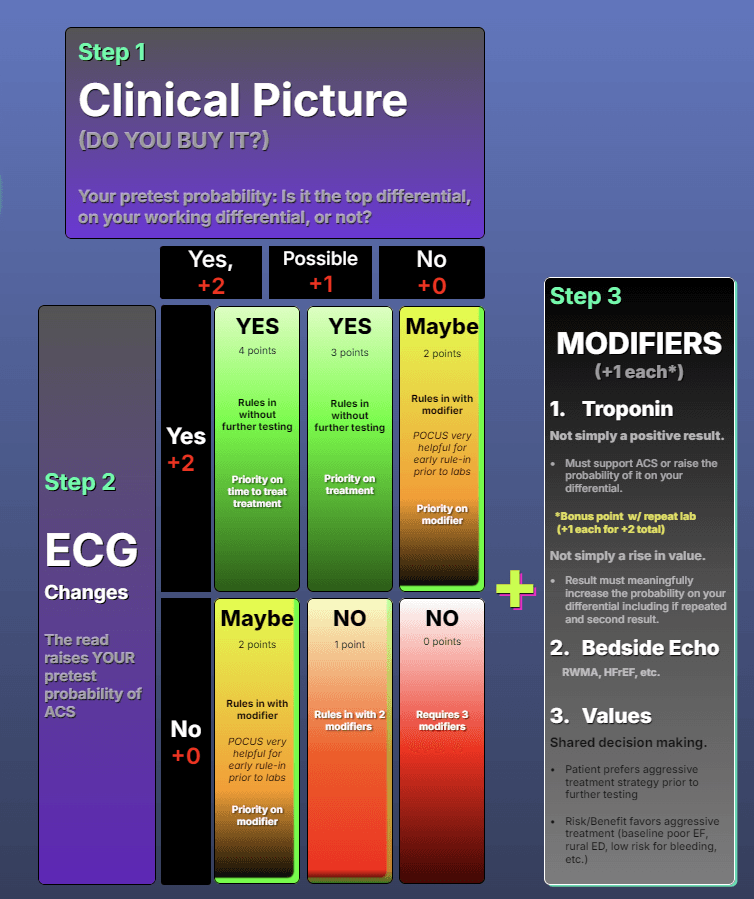
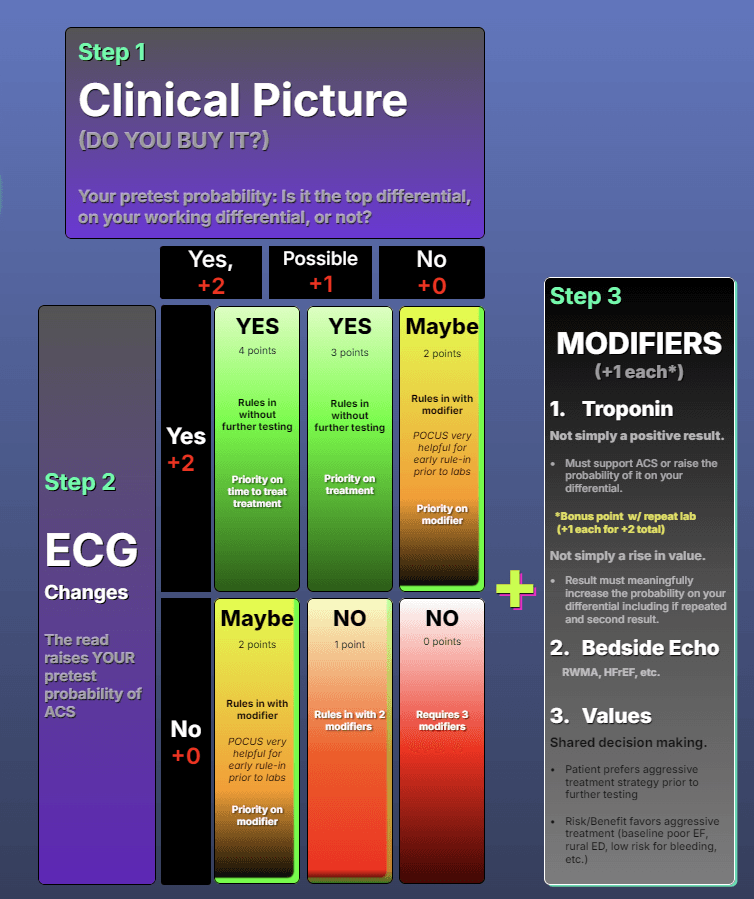
Step 1
Clinical Picture
(DO YOU BUY IT?)
Your pretest probability: Is it the top differential, on your working differential, or not?
Yes,
+2
Possible
+1
No
+0
Step 2
ECG Changes
The read raises YOUR pretest probability of ACS
Yes
+2
No
+0
YES
4 points
Rules in without further testing
Priority on time to treat
YES
3 points
Rules in without further testing
Priority on treatment
Maybe
2 points
Rules in with modifier
POCUS very helpful for early rule-in prior to labs
Priority on modifier
Maybe
2 points
Rules in with modifier
POCUS very helpful for early rule-in prior to labs
Priority on modifier
NO
1 point
Rules in with 2 modifiers
NO
0 points
Requires 3 modifiers
+
Step 3
MODIFIERS
(+1 each*)
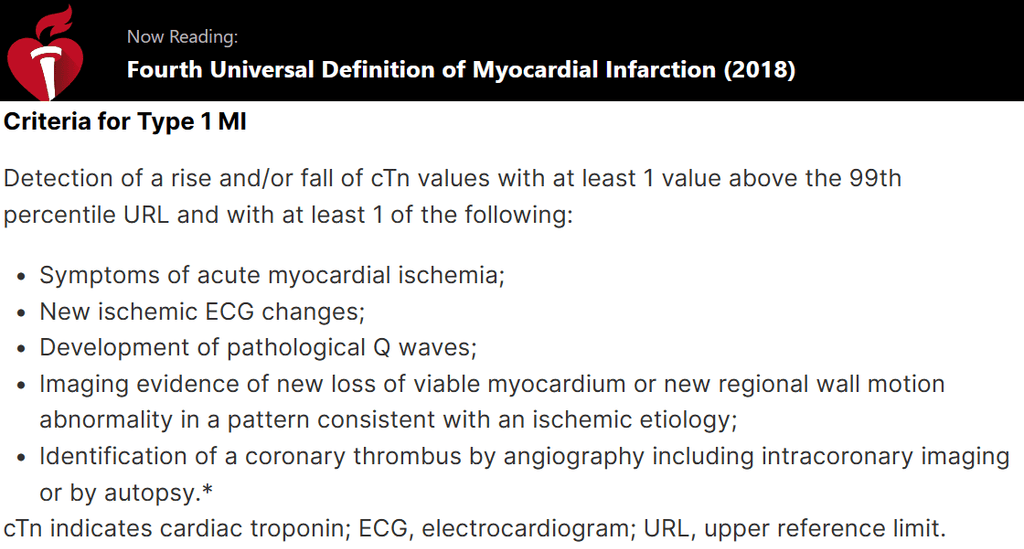
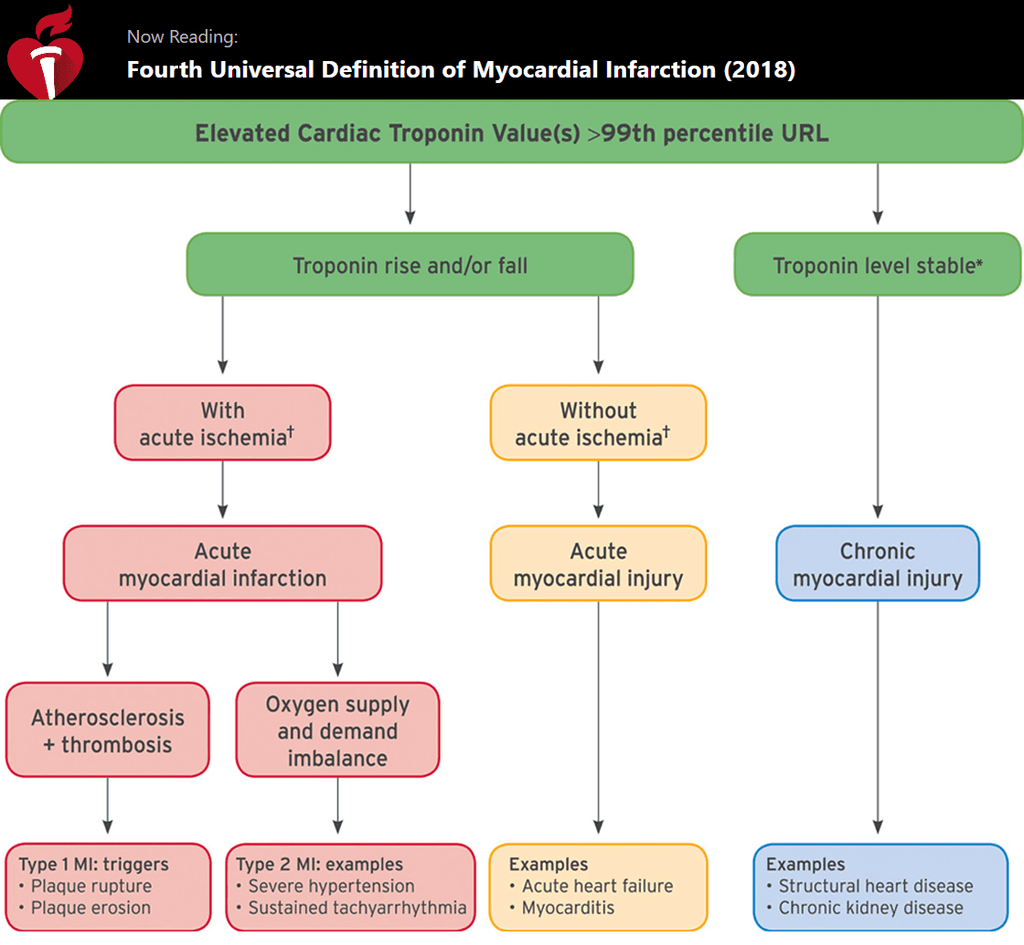
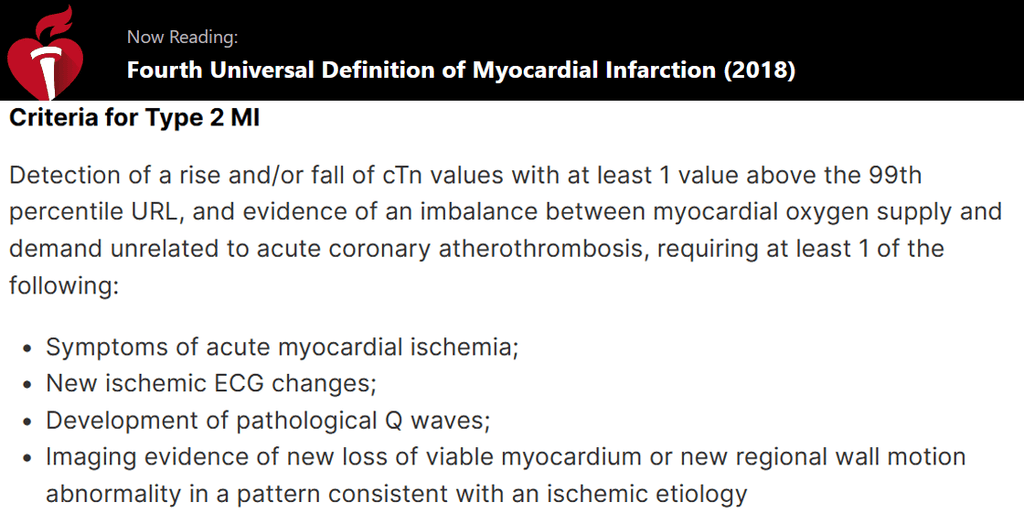
Troponin
Not simply a positive result.
Must support ACS or raise the probability of it on your differential.
*Bonus point w/ repeat lab
(+1 each for +2 total)
Not simply a rise in value.
Result must meaningfully increase the probability on your differential including if repeated and second result.
Bedside Echo
RWMA, HFrEF, etc.
Values
Shared decision making.
Patient prefers aggressive treatment strategy prior to further testing
Risk/Benefit favors aggressive treatment (baseline poor EF, rural ED, low risk for bleeding, etc.)
25 yo F w/ textbook vasovagal syncope at restaurant and reassuring ecg has unexpectedly positive hs troponin.
Step 1: 0 Step 2: 0 Modifier: 1
Total: 1
Without change in clinical picture/ecg this scenario would require 2 or more modifiers to treat as ACS.65 yo F hx of COPD presents SOB. ECG unchanged from prior. Troponin elevated without alternative explanation.
Step 1: 1 Step 2: 0 Modifier: 1
Total: 2
Without change in clinical picture/ecg this scenario would require a single modifier to treat as ACS.55 yo M hx of hypertrophic cardiomyopathy bibems c/o SOB.
v/s: T: 103 HR: 140 SpO2: 78 BP: 220/120
ECG reassuring. Echo reassuring. Troponin neg. Troponin #2: mild elevation.
Step 1: 1 Step 2: 0 Modifier: 0
Total: 1
Explanation: Troponin in range expected given hx HCM and v/s.
Without change in clinical picture/ecg this scenario would require 2 or more modifiers to treat as ACS.
55 yo M hx of hypertrophic cardiomyopathy bibems c/o SOB.
v/s: T: 103 HR: 140 SpO2: 78 BP: 220/120
ECG reassuring. Echo reassuring. Troponin neg. Troponin #2: mild elevation.
Step 1: 1 Step 2: 0 Modifier: 0
Total: 1
Explanation: Troponin in range expected given hx HCM and v/s.
Without change in clinical picture/ecg this scenario would require 2 or more modifiers to treat as ACS.65 yo F hx of COPD presents SOB. ECG unchanged from prior. Troponin elevated without alternative explanation.
Step 1: 1 Step 2: 0 Modifier: 1
Total: 2
Without change in clinical picture/ecg this scenario would require a single modifier to treat as ACS.25 yo F w/ textbook vasovagal syncope at restaurant and reassuring ecg has unexpectedly positive hs troponin.
Step 1: 0 Step 2: 0 Modifier: 1
Total: 1
Without change in clinical picture/ecg this scenario would require 2 or more modifiers to treat as ACS.
Examples
Examples
See the calculator at work for various clinical scenarios.
See the calculator at work for various clinical scenarios.
Impetus
All too often an ACS workup seems to hinge on single lab result, the troponin. However, even the latest generation of cardiac enzymes has not changed the foundation of clinical diagnosis in conjunction with ecg.
While the term myocardial injury has been introduced the "NSTEMI" diagnosis is still frequently misapplied—even in patients whose clinical presentation is incompatible. Conversely, the patient with an OMI whom presented with ecg changes (such as hyperacute t waves) alongside a concerning history may have care delayed or hindered if their first lab result is deemed unimpressive.
Curiously, this is often with the same physicians who voice subscription to the now ascending OMI paradigm (1) (2).While the inspirational work of Dr. Smith and others has made it plain to see the merit of moving beyond NSTEMI / STEMI paradigm the path for HOW remains less clear.
By consistently assuming the responsibility for diagnosis and treatment of ACS via the calculator pathway often little resistance is encountered even without classic STEMI symptoms. This tool is a foundational model to grow but if successful the aspiration is to grow beyond ACS rule in and assist with OMI rule in.
This calculator helps give the groundwork to consistently and logically diagnose and treat ACS while emphasizing the most important tests and interaction with patient.
The origin of this calculator is a direct result of experiences training residents puzzled at aggressive treatment despite, or prior to, the all important troponin result.
There is a real danger with so many pressures on the emergency physician to grind the specialty down to a "triage specialist" whose role is to brainlessly consult for the go ahead to treat the most obvious of cases or due to a spurious lab result.
I firmly believe initial ACS management is best performed by the most experienced specialty who is bedside with the patient: the emergency physician. While our cardiology colleagues are are an invaluable asset and part of the team to be utilized when necessary. The aim of this tool is to foster similar ownership and confidence in others whom use it.
All too often an ACS workup seems to hinge on single lab result, the troponin. However, even the latest generation of cardiac enzymes has not changed the foundation of clinical diagnosis in conjunction with ecg.
While the term myocardial injury has been introduced the "NSTEMI" diagnosis is still frequently misapplied—even in patients whose clinical presentation is incompatible. Conversely, the patient with an OMI whom presented with ecg changes (such as hyperacute t waves) alongside a concerning history may have care delayed or hindered if their first lab result is deemed unimpressive.
Curiously, this is often with the same physicians who voice subscription to the now ascending OMI paradigm (1) (2).While the inspirational work of Dr. Smith and others has made it plain to see the merit of moving beyond NSTEMI / STEMI paradigm the path for HOW remains less clear.
By consistently assuming the responsibility for diagnosis and treatment of ACS via the calculator pathway often little resistance is encountered even without classic STEMI symptoms. This tool is a foundational model to grow but if successful the aspiration is to grow beyond ACS rule in and assist with OMI rule in.
This calculator helps give the groundwork to consistently and logically diagnose and treat ACS while emphasizing the most important tests and interaction with patient.
The origin of this calculator is a direct result of experiences training residents puzzled at aggressive treatment despite, or prior to, the all important troponin result.
There is a real danger with so many pressures on the emergency physician to grind the specialty down to a "triage specialist" whose role is to brainlessly consult for the go ahead to treat the most obvious of cases or due to a spurious lab result.
I firmly believe initial ACS management is best performed by the most experienced specialty who is bedside with the patient: the emergency physician. While our cardiology colleagues are are an invaluable asset and part of the team to be utilized when necessary. The aim of this tool is to foster similar ownership and confidence in others whom use it.
The ideal physician…
is a thinking physician
The ideal physician
Diagnoses and treats ACS proactively rather than reactively.
Prioritizes real-time bedside evaluations and clinical picture.
Confidently assumes ultimate responsibility for initial workup, management, and diagnosis with patient buy-in.
Click on any heading to expand context